Hemorrhagic (red) Infarcts develop only in certain organs and under certain circumstances.
- ORGANS WITH DUAL BLOOD SUPPLY
The peculiarities of the blood supply of the lung and the liver consist in the presence of functional and nutritional blood vessels that bring blood into the microcirculation (capillaries of these organs) and main venous vessels that take blood away from them. In the lung enters the pulmonary artery (functional vessel), which carries venous blood from the right heart chamber, and the bronchial artery, which supplies oxygen and nutrients to the tissues of the walls of the bronchi of different calibers. In the liver enters the portal vein (functional vessel), which carries blood from the stomach, intestines, spleen, and the hepatic artery, which supplies oxygen and nutrients to the hepatocytes. Due to the presence of two vessels that bring blood to these organs, the blockage of one of them by a thrombus or embolus does not lead to a complete stoppage of blood flow and therefore does not follow a infarct (necrosis), because absolute ischemia does not occur. However, when obstruction of the functional blood vessel develops against the background of severe chronic venous congestion, then the nutrient vessel, which has a much smaller flow rate, cannot resist the high pressure in the venous part of the circulation, and a hemorrhagic infarction occurs.

A classic example is the hemorrhagic infarct of the lung. A prerequisite for its occurrence is the presence of chronic venous congestion in the organ caused by valvular disease (mitral stenosis) or chronic left-sided heart failure, a consequence of CHD (chronic ischemic heart disease). In these cases, the morphological picture of chronic venous congestion in the lung is Brown induration (macroscopically) or Hemosiderosis (microscopically). If a thromboembolism occurs in one of the segmental branches of the pulmonary artery in such a lung, then the bronchial artery cannot „push“ the blood against the high pressure in the branches of the pulmonary veins. The movement of blood stops, i.e. absolute ischemia and necrosis develop in the lung parenchyma, including in the walls of blood vessels. The walls of the capillaries and venules rupture and the alveoli fill with blood. The spongy loose structure of the lung parenchyma collects a large amount of blood and a hemorrhagic infarct occurs, which over time becomes denser due to organization, and its violet color changes to rusty brown due to the formation of hemosiderin by macrophages. Microscopically, the air spaces in this area are filled with blood, and the lung parenchymal tissues are necrotic.
2. ORGANS WITH PLENTY OF ARTERIO-ARTERIAL ANASTOMOSES
Hemorrhagic infarcts of this type develop in the small intestine, when some of the branches of the mesenteric arteries are blocked by thrombi or emboli. The final branches of these arteries have a large number of anastomoses in the area of the arcades. When these branches are blocked, there are no disturbances in blood supply, because the intestinal wall receives blood from the anastomoses as well. However, if a major branch of the mesenteric artery supplying a large segment of the small intestine is occluded, these anastomoses cannot compensate for the lack of blood in the intestinal wall. They slowly fill the anemic area, the small vessels overflow with blood, but it stops moving due to the lack of the push wave from the main artery. Capillaries and venules are thin-walled, rupture, and blood permeates the loose tissues of the necrotic intestinal wall. It swells, becomes dark red-black and a hemorrhagic infarction develops.

3. OBSTRUCTION OF LARGE ORGAN VEINS WITHOUT ANASTOMOSES
Obstruction of collateral-free large organ veins results in complete blockage of blood flow. The increase in pressure in the circulatory system also blocks the flow of arterial blood. By this mechanism, hemorrhagic infarction in the ovary can develop. The trunk arteries and veins of this organ pass through the mesovarium. Torsion of the ovary around the mesovarium leads to cessation of blood flow through the thin-walled ovarian vein, with subsequent severe venous stasis, dilatation and rupture of venules and capillaries, permeation of tissues with blood, and cessation of arterial flow due to increased pressure in this area. Absolute ischemia develops resulting in a hemorrhagic infarction. This group of hemorrhagic infarcts also includes the small intestine. Thrombosis of a mesenteric vein by the same mechanism leads to impregnation of the intestinal wall with blood, with subsequent cessation of arterial blood flow and the development of a infarction, which is hemorrhagic. Due to the sequence of the processes – first perfusion with blood due to blocking of the venous outflow and then – the absolute ischemia with the infarct, the correct diagnosis in this case is „Hemorrhagic infarct“ of the small intestine. The clinical picture is dramatic – on a sharp abdomen and during the operation surgeons see dark red-black necrotic intestinal loops. If only part of the small intestine is involved, it is possible to surgically excise the dead tissue and save the patient. In severe cases of massive hemorrhagic intestinal infarction, the outcome is usually fatal. Then the surgeons are difficult to assess the exact cause of the infarction – thromboembolism of the mesenteric artery or thrombosis of the mesenteric vein. In the first case, it concerns a real hemorrhagic infarct, in the second – a drenching with blood of the intestinal wall. The surgeons get out of this difficult diagnostic situation with the summary diagnosis „Mesenteric thrombosis“, without specifying which blood vessel is blocked – artery or vein.
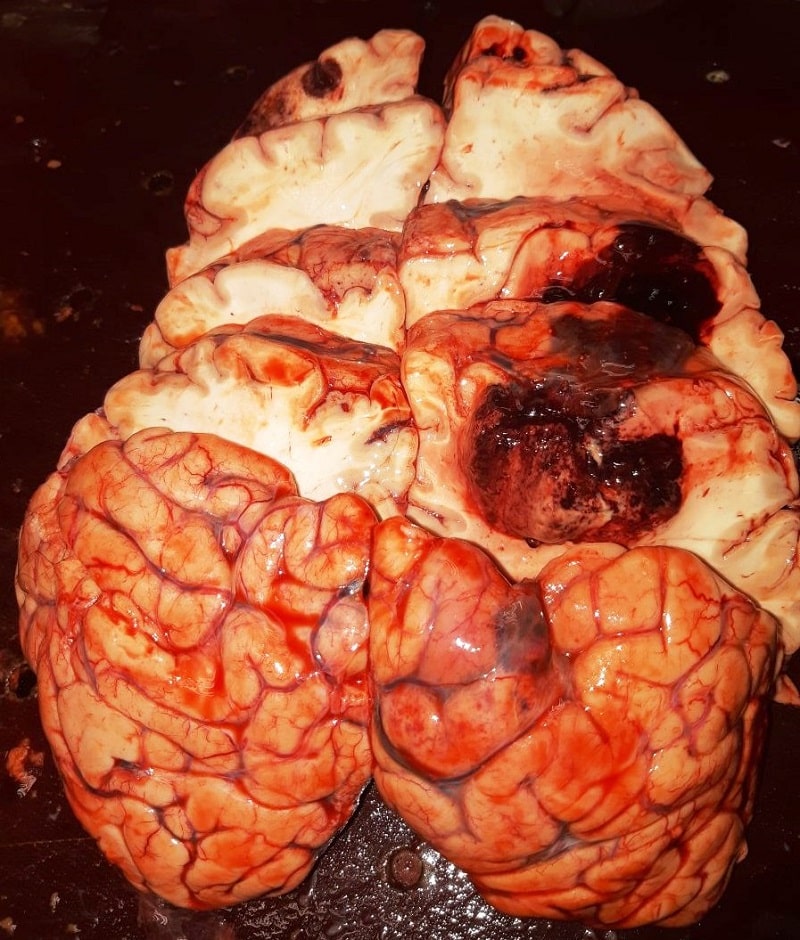
4. HEMORRHAGIC CEREBRAL INFARTION (Red brain softening)
This type of hemorrhagic infarct develops in two stages. It begins with an embolic blockage of a large cerebral artery. This causes anemic brain infarction with the development of liquefactive necrosis. At the next stage, the thromboembolism can be destroyed by the fibrinolytic system and small fragments of it can move further to the peripheral vascular branches. With the restoration of blood flow through the main blood vessel, the walls of which are also necrotic, blood flows through them to the outside. Hemorrhage floods the necrotic brain tissue and the infarct changes from ischemic to hemorrhagic.
